Not all patients require treatment. It is necessary to treat when spasticity induces deformities or functional impairment.
The care of spastic patients is best organized as a team work around the patient and family, including all the professionals involved in the treatment: family doctor or pediatrician, neurologist, physiatrist, physiotherapist and occupational therapist, and surgeon…
This is usually a long term treatment and participation of the patient and his family is paramount.
Physical and occupational therapy.
Physical and occupational therapy are initiated early.
Physical therapy aims at keeping the spastic muscles supple and avoiding muscle contracture, as well as exercising weak or paralysed muscles in order to reinforce them. The goal is to prevent deformities and muscle contractures.
Occupational therapy aims at stimulating the use of all muscles, whether spastic or weak, in order to maintain as much function as possible despite the deficit. Bimanual activities are encouraged: pencil and ruler, carrying a tray, bicycle, swimming, bimanual games (computer games, Russian dolls…).
Constraint-induced movement therapy consists in preventing the use of the contralateral normal hand, by fitting it with a splint or a glove, in order to make the patient use exclusively his: her spastic hand. Protocols often involve the CIT therapy three to four hour a day for three to four week periods.
Electrical stimulation (myo feed-back) of the weak or paralysed muscles may help to reinforce these muscles.
Splints
Splints are used in adjunction to physiotherapy, in order to prevent deformities, or to treat them when they are present. They are worm mostly at night, but day splints may be necessary in some cases.
Splints and orthosis must be costum-made in order to be comfortable. A splint which causes pain or skin irritation is likely to produce the opposite effect, i.e. to increase the spasticity. They must be regularly checked, especially in the growing child.
Anti-spasmodic medications
Several medications are effective on spasticity. Some are administered orally, some directly into the nervous system, and some locally, into or near the spastic muscle.
When there is diffuse spasticity (severe CP) medications such as baclofene, dantrolene or gabapentine are helpful. But sometimes side effects prevent their use.
They can be administered orally, or intra-thecally in contact with the nervous system. Implanted pumps can deliver a fixed amount of medication each day, for a long term effect.
Some medications can be administered locally, into a spastic muscle or its motor nervesNerve branch enering a muscle and giving it the “command” to contract. All muscles have their own motor branch(es).. They aim at reducing the motor tone of the muscle. Their effect is only temporary. There are two types of local medications:
- botulinum toxin prevents the nerve impulse from being delivered to the muscle, by blocking the release of a substance (acetylcholine) which normally causes the muscle to contract. There are two main brands of botulinum toxin available for clinical use: Dysport ®, and Botox ®.
The target muscle is identified, usually with electro-stimulation or ultra-sounds. Then botulinum toxin is injected directly into the muscle via a syringe and a needle. In children it can be administered under sedation.
Its effect on the muscle starts after a few days, and lasts three to five months. During this period, the physical therapy is reinforced on the non spastic (antagonist) muscles, and splints may be indicated to fight deformities. This is reversible: spasticity returns as soon as the effect of the treatment has ceased.
It is indicated when a muscle becomes so spastic, despite all other treatments, that it impairs function, or nursing, or creates pain. It is also used in the planning of surgical treatment both for decision making, and for helping the patient to visualize what benefit he/she can gain from surgery.
- motor blocks are used nowadays mostly when botulinum is not available; They consist in injecting a substance (local anesthetics, alcohol, or phenol) around the motor nerve*, which blocks the nerve impulse and paralyses the muscle temporarily. The duration of the paralysis depends on the injected substance (one hour for local anesthetics, several weeks for phenol).
Assessments
Regular evaluations are performed, in order to assess the status of the upper imb, and the short and long term benefit of any treatment, They involve clinical evaluation of spasticity, muscle strength, joint stiffness (muscle / joint contracture), and sensation.
A number of tests exist in order to evaluate the function of the hand, for example:
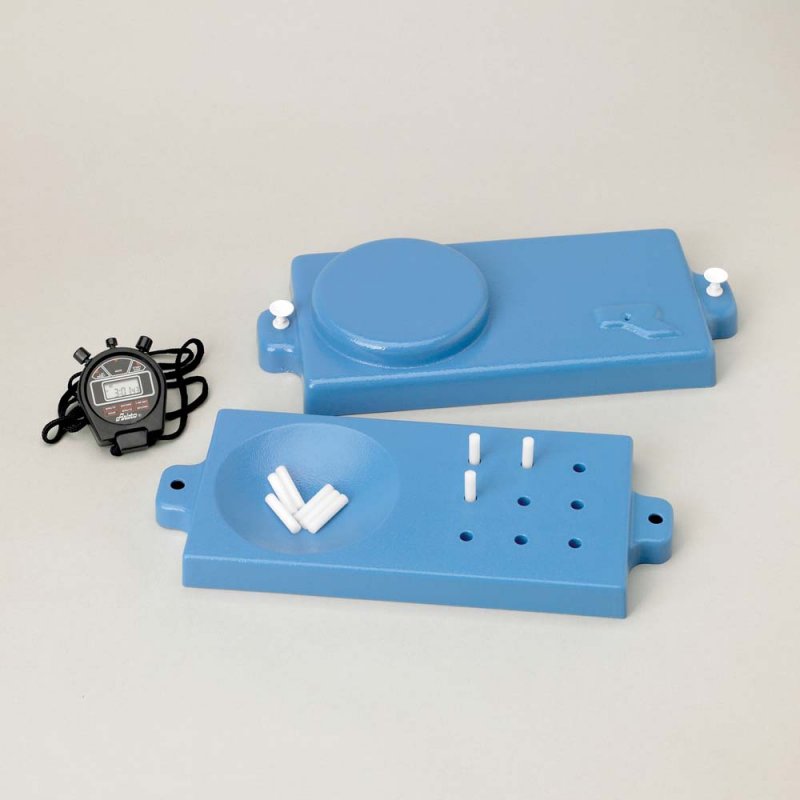
| the box and blockTest de dextérité manuelle standardisé et chronométré consistant à transférer le maximum de cubes de bois d’un côté à l’autre d’une boîte en bois et un temps donné. test | the nine hole peg Test de dextérité manuelle fine, standardisé et chronométré, consistant à prendre des petits cylindres de bois et à les insérer dans les orifices correspondants sur une tablette.test |
 |
 |
Also a number of assessments, scales and classifications are used, some of which have been specifically designed for the spastic upper limb. (AHA, Melbourne, SHUUE…)
The HOUSE classification is a simple and effective way to describe the gross function of the hand:
|
Grade |
Designation |
Activity level |
|
0 |
Does not use |
Does not use |
|
1 |
Poor passive assist |
Uses as stabilizing weight only |
|
2 |
Fair passive assist |
Can hold on to object placed in hand |
|
3 |
Good passive assist |
Can hold on to object and stabilize it for use by the other hand |
|
4 |
Poor active assist |
Can actively grasp object and hold it weakly |
|
5 |
Fair active assist |
Can actively grasp object and stabilize it well |
|
6 |
Good active assist |
Can actively grasp object and then manipulate it against other hand |
|
7 |
Spontaneous use, partial |
Can perform bimanual activities easily and occasionally uses the hand spontaneously |
|
8 |
Spontaneous use, complete |
Uses hand completely independently without reference to the other hand |
House functional classification






