Abnormal movements
Abnormal movements, also referred to as “movement disorders”, occur involontarily and out of the patient’s control. They can occur at rest or during activity. In spastic patients, the most frequent abnormal movements are:
-dystonia, characterized by sustained muscle contractions cause twisting and repetitive movements or abnormal postures. Dystonia is often initiated or worsened by voluntary movements, and seems due to a lack of motor coordination (lack of reciprocal inhibition of agonist / antagonist muscles). In the upper limb it often produces abnormal postures in ulnar deviation of the wrist, and in finger extension when the wrist is flexed. Severe dystonia is a contra-indication to surgery.
- chorea is made of brief, semi-directed, irregular movements that are not repetitive or rhythmic, but appear to flow from one muscle to the next ('dance-like' movements).
- athetosis is characterized by slow, involuntary, convoluted, writhing movements of the fingers, hands, toes, and feet and in some cases, arms, legs, neck and tongue. It can be quite permanent, ceasing only during sleep.
Agonist / Antagonist muscle
A muscle which produces the opposite movement. Example wrist extensors are antogonist of wrist flexor.
Block and box test
Standardized manual ability test consisting in transferring the maximum number of wooden squares from one side of a box to the other in a set time.
Cerebral Palsy (CP)
Cerebral palsy is a neurological disorder caused by a brain injury or malformation that occurs while the child’s brain is under development (foetus and infant). These non-progressive lesions affects body movement, posture and muscle coordination, and cause limb deformities and functional impairment.
Clonus
A clonus is a series of involuntary rhythmic muscle contractions. Unlike abnormal movements, it does not occur spontaneously, but is initiated by a reflex.
Co-contraction
It is the inappropriate recruitment of a muscle upon activating the muscle producing the opposite movement (antagonist). Example: co-contraction of the triceps when activating the biceps prevents flexion of the elbow.
Hemiplegia
Paralysis affecting one side of the body (upper and lower limb).
Motor nerve
Nerve branch enering a muscle and giving it the “command” to contract. All muscles have their own motor branch(es).
Muscle tone
Muscle tone is the continuous and passive part of contraction of the muscles. It helps to maintain posture and fight gravity at rest, and declines during sleep.
Hypertonia is a pathological increase of tonus resulting from an upper motor neuron disease. It can present clinically as either spasticity or rigidity. While spasticity results from a lesion of the pyramidal tract (lesion of the brain or the spine), rigidity is a consequence of a lesion of the extra-pyramidal tract (ex: Parkinson).
Hypertonia is a pathological increase of tonus resulting from an upper motor neuron disease. It can present clinically as either spasticity or rigidity. While spasticity results from a lesion of the pyramidal tract (lesion of the brain or the spine), rigidity is a consequence of a lesion of the extra-pyramidal tract (ex: Parkinson).
Nine hole peg test
Standardized and time-recorded test of fine manual ability consisting in taking small wooden cylinders from a container, and introducing them in fitted holes in a tablet.
Pronator / supinator muscles
With the elbow flexed, pronators muscles rotate the hand palm down, whereas the supinators bring the palm upwards.
Quadriplegia
Paralysis of all four limbs.
The stretch reflex (“myotatic reflex”) is an automatic (or “reflex”) muscle contraction in response to an unexpected stretching within the muscle. It is sought for during every neurological examination. The most known reflex is the patellar reflex (“knee-jerk): with the knee flexed and the thigh muscles relaxed, percussion of the patellar ligament causes leg extension by reflex contraction of the quadriceps muscle.
Stretch reflexes are exagerated in brain and spine lesions, especially in spasticity.
Stretch reflexes are exagerated in brain and spine lesions, especially in spasticity.
Stroke
Stroke, also known as cerebrovascular accident (CVA), or brain attack, is a neurologic condition due to a sudden decrease of blood flow to the brain, resulting in cell death. There are two main types of stroke: ischemic due to lack of blood flow and hemorrhagic due to bleeding.
Symptoms of a stroke may vary greatly form one patient to the other, depending on its nature (ischemic or hemorrhagic), and on the location and the size of the brain lesion.
Signs and symptoms often appear within minutes after the stroke. In some cases, they last less than one or two hours, it is then known as a transient ischemic attack (TIA). In other cases, they can be permanent.
In occidental countries, one in 600 persons sustain a stroke each year. 80% are ischemic, and 20% hemorrhagic. The chance to sustain an ischemic stroke increases with age, whereas the chance to sustain an hemorrhagic one is independent of age.
Symptoms of a stroke may vary greatly form one patient to the other, depending on its nature (ischemic or hemorrhagic), and on the location and the size of the brain lesion.
Signs and symptoms often appear within minutes after the stroke. In some cases, they last less than one or two hours, it is then known as a transient ischemic attack (TIA). In other cases, they can be permanent.
In occidental countries, one in 600 persons sustain a stroke each year. 80% are ischemic, and 20% hemorrhagic. The chance to sustain an ischemic stroke increases with age, whereas the chance to sustain an hemorrhagic one is independent of age.
upper motor neuron lesion
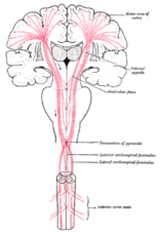 Lesion of the neural system above the anterior horn cell of the spinal cord (in contrast to a lower motor neuron lesion, which affects nerve fibers traveling from the anterior horn down to the relevant muscles). These are the neural fibers carrying signals for voluntary movement of skeletal muscle. They usually originate in the primary motor cortex, cross over to the opposite side (decussation), and proceed down the spinal cord to meet lower motor neurons in the anterior horn.
Lesion of the neural system above the anterior horn cell of the spinal cord (in contrast to a lower motor neuron lesion, which affects nerve fibers traveling from the anterior horn down to the relevant muscles). These are the neural fibers carrying signals for voluntary movement of skeletal muscle. They usually originate in the primary motor cortex, cross over to the opposite side (decussation), and proceed down the spinal cord to meet lower motor neurons in the anterior horn.





